Blog Post
Alyson Prince • 27 May 2021
Lonely Infection Control Nurse – Seeks Voice
COVID has focused the minds of many around how Infection Control is managed in the hospital environment

I have been in this role since 2011, saying all the things people are saying now, how do we manage the transmission of infection in the hospital environment more effectively. Its like the saddest game of I told you so. In my role I noted how important it is to have IPC involved from the beginning, even in meetings where clinical teams meet, it is important to have IPC representation. It helps inform infection risk assessment from the beginning to lessen the risk of serious and costly mistakes, from a financial and patient safety perspective.
As one of the only nurses doing this role, I was placed between the two departments, the building/estates departments and the IPC teams, building relationships as much as anything else, and going on a steep learning curve. I trouble shoot theatre ventilation when it fails, went to already started projects where it was clear that the person that signed them off didn't understand the engineering and the engineers didn't understand the clinical aspects of the project.
However it may surprise you that there is no formal education programme
infection control nurses can undertake to become proficient in this role.
One of the things I have always struggled is perception. It has been since the beginning and remains very difficult to define what my role is and how quantifyingly valuable it is. Many clinical teams view me as an infection control nurse, and don't understand I have this remit, so have separate discussions about their areas and don't consider infection control forms part of the risk assessment that is required to ensure that clinical activity is safe, and there are many examples of this.
In terms of the healthcare planning and design team, they often disregard infection control as an expensive annoyance which increases the cost of the project. They can also see it as restrictive to the development and delivery of modern spaces which they aim to design to improve patient experience. Each aspect has its own value, and it is a decision to understand which risk is higher.
Infection control is often juxtaposed with other constraints such as cost, environmental impact, clinical activity ever expanding services requiring more and more patient space and ever increasingly complex and changing care delivery and invasive procedures.
From concept through to completion, it is a complex decision process understanding the requirements and trying to future proof the spaces.
One thing that needs to be understood is that the building is a whole system, the mechanical systems are all interlinked, so how it is designed for one space, wont necessarily work in another space. Both air and water systems similar to electrical systems are fixed systems, the issue with that is that the air and water systems can also support and introduce organic growth, and provide a source of opportunistic infection so it needs to be understood when the building is operational that changes to the building will impact the growth in the system. When the use of an area is inappropriate then it will be impacted in its safety, we need to start educating healthcare workers on the use of the building during their training, so they understand the relationship to the unit they are working in has to the building and what their actions will do.
When this goes wrong, it can cause patient safety issues and often costs more than the original outlay of the build and the operational. It is not just the planning and design that can influence the spread of infection control practice often can impact on spread of infection also. The practice of placing hand wash basins in each bed space to encourage hand hygiene at the point of care, often leaves the bed space open and therefore if there is no-one using the space, then this in effect a dead leg and supports biofilm development.
Further to this, if the outlet is not maintained appropriately then this can support the growth of pseudomonas which can be transferred on the hands of staff to patients, as has been widely documented and resulted in a re-write of the HTM guidance to improve management and maintenance of the outlet. Patients who occupy single rooms, often have en-suites that they are too sick to use, leaving it as a little used outlet and can influence the growth on that run, as these often tend to be located alongside each other due to space constraints.
This highlights the complex relationship between the building design and infection. Hospitals have subsequently demonstrated a relationship between outbreaks of multi-drug resistant organisms originating from ITU outlets where the clinical staff cant leave the patient, they often use the HWB for other uses, such as tipping wash-water down the sink, without a second thought, not knowing that they could be potentially contaminating that outlet with the organisms from the patients.
How do we resolve these issues? There is an answer and in short it is education. We need to expand the education of the infection control nurses of the future and show them that there is a whole specialist area allocated to the environment that continues way beyond completion Each clinical area has specific requirements and we need to educate engineers in the new and emerging pathogens which pose a risk to our patients, not tell them that it isnt for IPC to engineers
From water, to air, from surfaces, to space allocation, all of these things interplay with each other and require to map the clinical activity to the space. It is harder to design a space without understanding the clinical activity, and therefore requires clear, consistent and informed discussions
We couldnt discuss planning without discussing refurbishment and upgrade. It is varied in the quality of delivery, from design brief, to delivery and the existing infrastructure can also play a part. We need to remember some hospitals are often hundreds years old, with re-fashioned systems crammed in to ensure compliance, but there is usually a connection with the old infrastructure and the new, and this can pose big risks,.. I am reminded of a time where an electrical panel was flooded as where it was located in the plant room meant that the water went downwards to the panel, and shut the hospital, you sometimes have to work with what you have and be pragmatic.
Much work needs to be undertaken with clinical designers and planners and infrastructure specialists, alongside bringing the guidance up to date with scientific discussion. This is no easy task, and is even more difficult to retrofit to updated standards as we are seeing with covid.
It is clear that this role is needed and I am grateful for all I have learned thus far, but still have a lot to learn, but also have a lot of learning to share, to help everyone have a better building to deliver the care our patients so deserve.
If you are interested in Infection Control in the Built Environment , please reach out to me on LinkedIn https://www.linkedin.com/in/alyson-prince-14793956
Email Us
For general enquiries & questions,
contact us via email
Book Free Consultation
Need some advice face to face? Book a free 30 minute MS Teams consultation
CHECK OUT OUR OTHER BLOG POSTS
Knowledge Hub

by Josie Winter
•
14 December 2023
This blog post delves into the findings of the "Global State of Patient Safety 2023" report by Imperial College London, exploring key aspects of patient safety around the world. It covers country-specific rankings, notable improvements, and areas of concern in healthcare systems. The post also highlights recommendations for future actions to enhance patient safety, emphasising the role of patient and family involvement, the importance of comprehensive data collection, and the need for global collaboration in healthcare improvement efforts.

by Josie Winter
•
13 November 2023
Explore the transformative journey towards healthcare excellence with our latest blog post, "Unlocking Excellence in Healthcare: A 7-Step Guide to Quality Care." This insightful post delves into the Health Foundation's adaptation of a Healthcare Quality Framework, presenting a comprehensive seven-step path designed to elevate the quality of care across the healthcare spectrum. From setting evidence-based priorities to embracing innovation and research, each step provides a strategic blueprint for healthcare professionals, organizations, and stakeholders to collaboratively enhance care quality. This guide is not just theoretical; it's a practical roadmap to close the care and quality gap, ensuring every patient receives the highest standard of care. Whether you're a healthcare provider seeking to improve patient outcomes or a stakeholder in the health sector, this blog post offers valuable insights and actionable strategies
by Josie Winter
•
14 October 2023
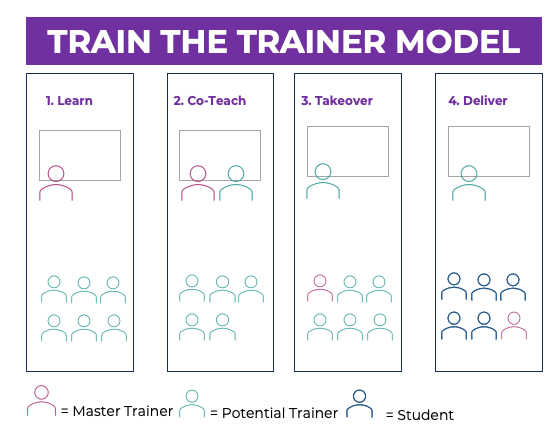
Train-the-Trainer (TTT) programs have emerged as a valuable strategy and cost effective way to enhance skills, knowledge, and performance among care professionals. These programs, however, come with their own set of benefits and risks. This article explores the advantages and potential pitfalls associated with TTT initiatives in the context of health and social care
by Josie Winter
•
24 August 2023
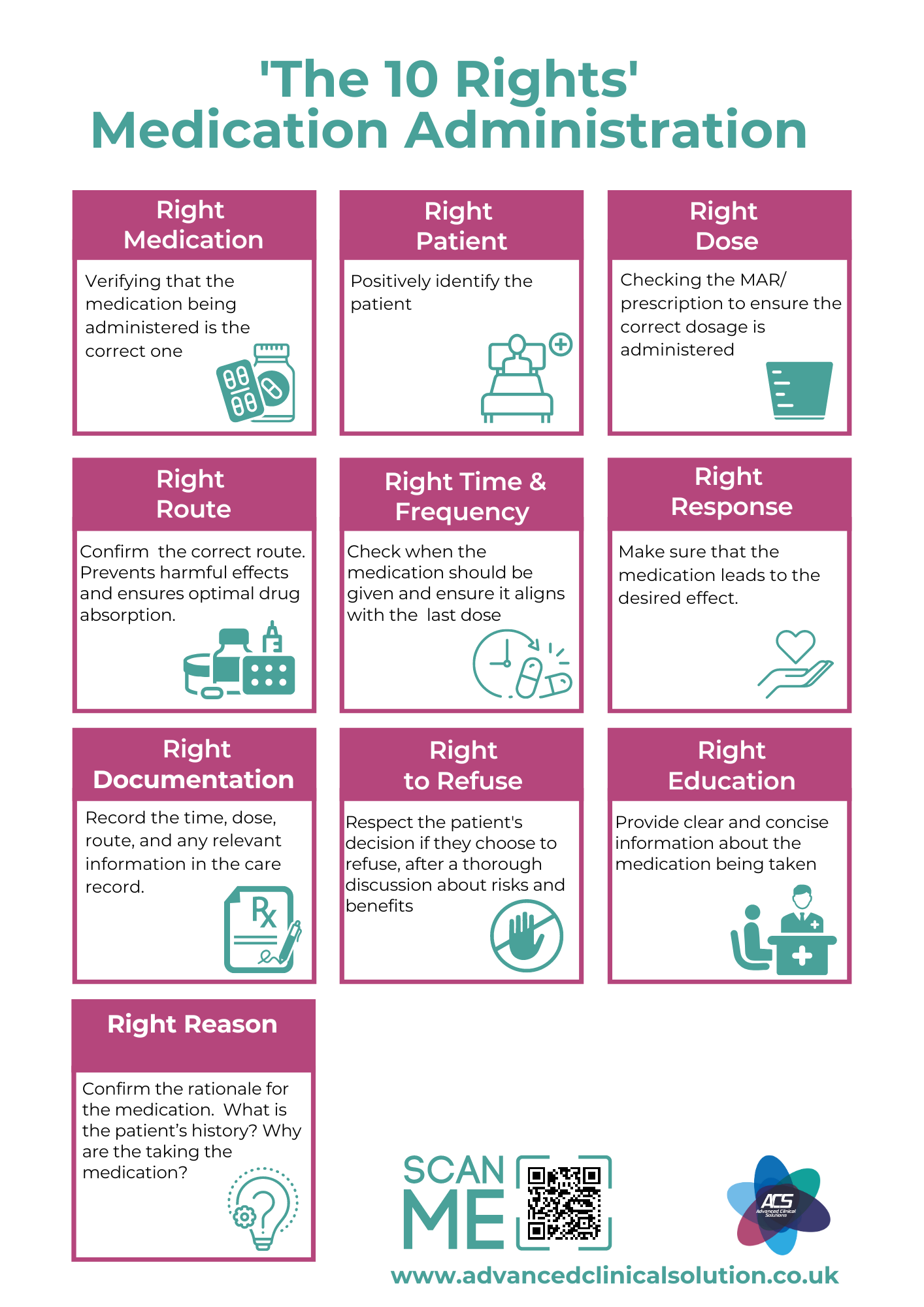
Mastering Medication Administration: Discover the 10 Rights for Medication Administration | Explore the comprehensive guide by Advanced Clinical Solutions, your trusted source for healthcare training. Elevate your expertise with our insightful blog post, delving into the crucial 10 Rights of Medication Administration. Learn how to ensure quality, safety, and patient well-being. Plus, don't miss our exclusive offerings – access FREE downloadable posters and specialized training resources on this essential topic. Enhance your skills today with Advanced Clinical Solutions!

by Josie Winter
•
17 August 2023
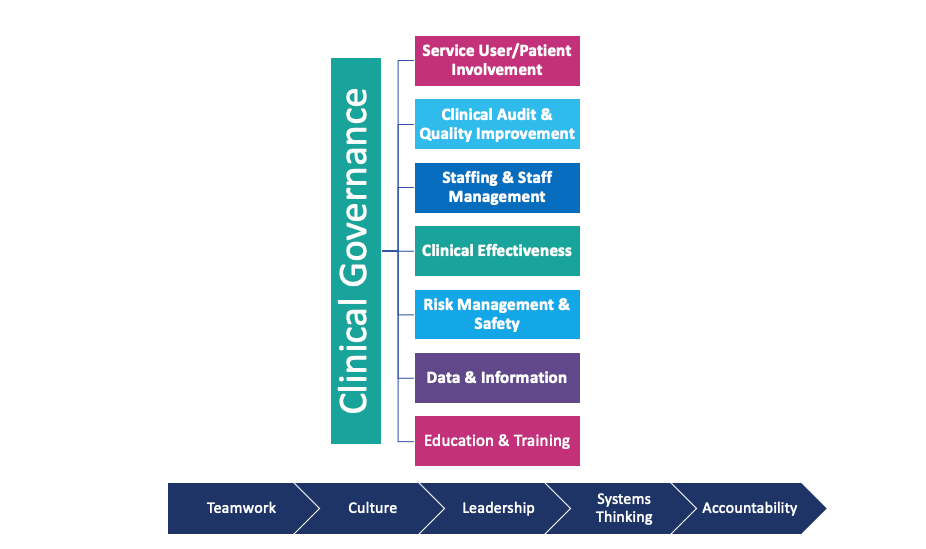
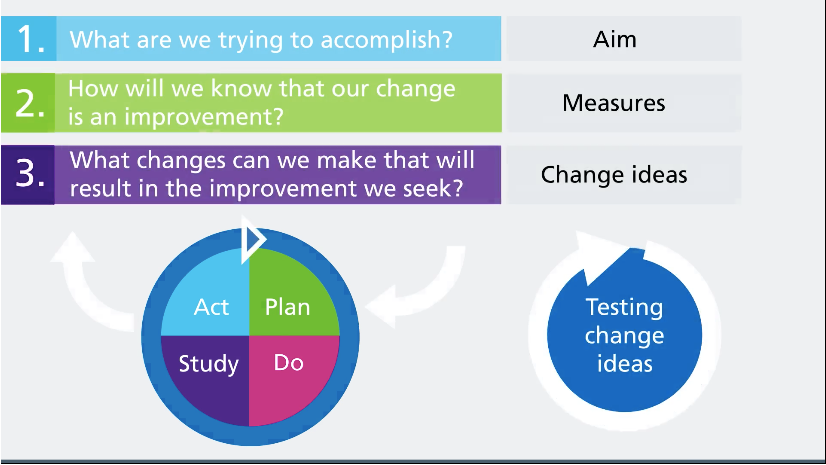
Elevating Care Standards: Bridging Healthcare Quality Improvement and Regulatory Compliance
High care standards are essential for ensuring that patients receive the best possible care. However, bridging the gap between care quality improvement and regulatory compliance can be challenging. This blog post discusses the importance of high care standards, the impact of regulatory compliance, and strategies for bridging the gap between these two important concepts.

4 August 2023
Discover how Advanced Clinical Solutions Ltd (ACS) is leading the way in improving quality and meeting CQC standards through staff training and development. This comprehensive blog post explores the crucial role of well-trained healthcare professionals in delivering high-quality patient care, boosting staff confidence, and ensuring compliance with CQC regulations. Learn how ACS offers tailored training programs, highly qualified trainers, and a comprehensive curriculum to empower healthcare organisations to succeed in the ever-evolving landscape of healthcare.

by Josie Winter
•
18 June 2023
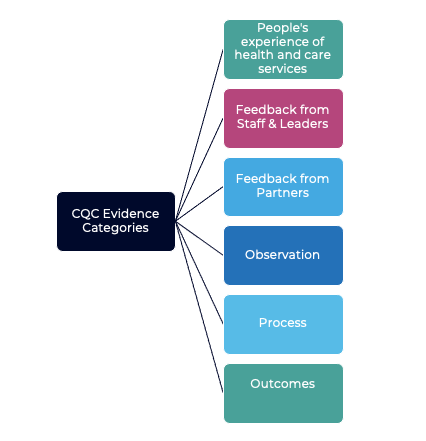
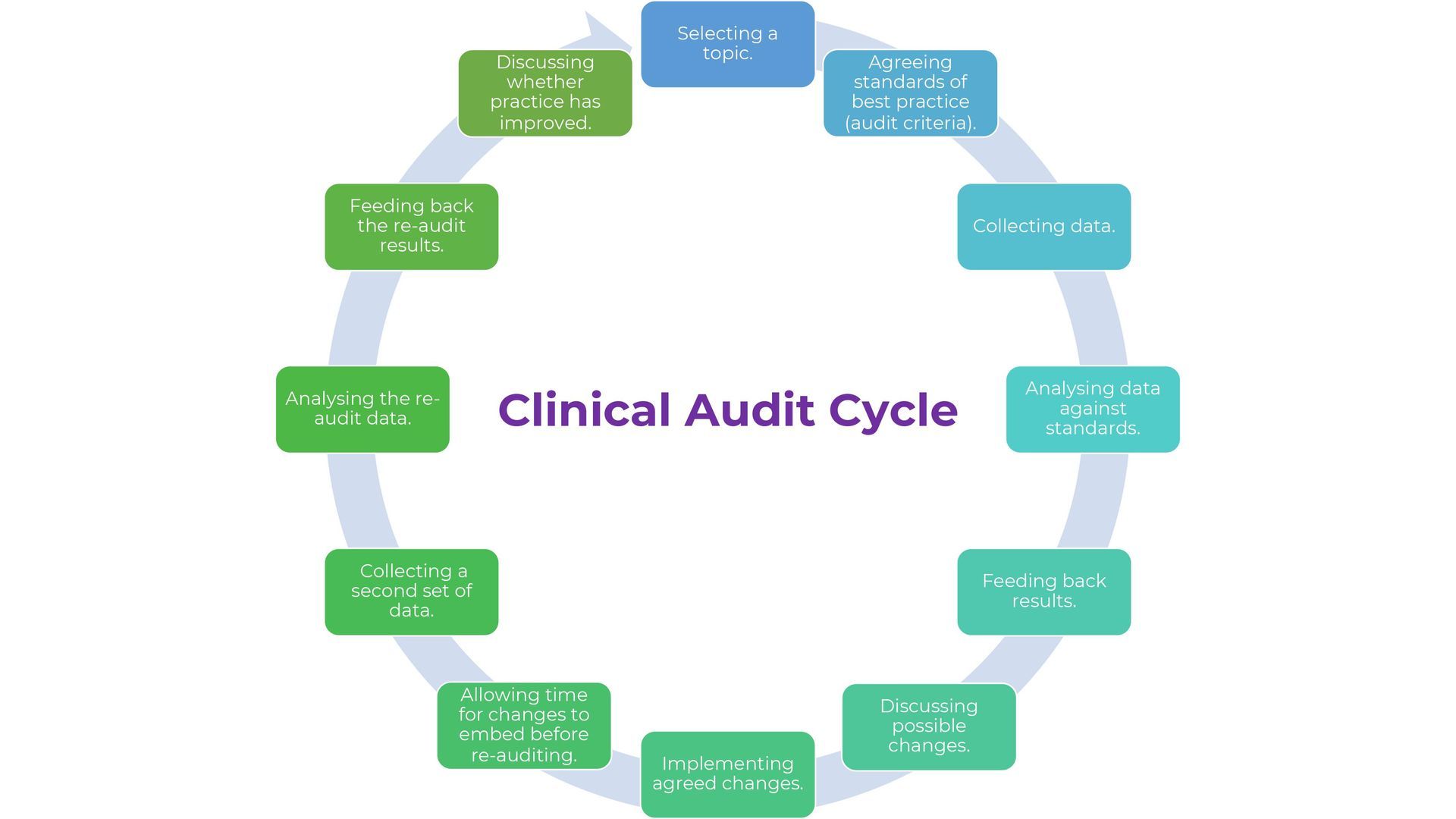
The Care Quality Commission (CQC) is responsible for regulating and inspecting healthcare providers in England to ensure that they provide safe, effective, caring, responsive, and well-led care. The CQC will be using a new single assessment framework (SAF) to assess the quality of care provided by these healthcare providers. In this blog post, we will explore the process of how the CQC reaches a rating under the new Single Assessment Framework.
Merlin House I Langstone Business Park
Newport I NP18 2HJ
Copyright © 2024 Advanced Clinical Solutions Ltd . All rights reserved
Company Reg : 10293607 VAT Reg: 290 6883 65