6 Questions to ask about Compliance & Quality Improvement.... that you should answer truthfully.
Gold Standard Practice
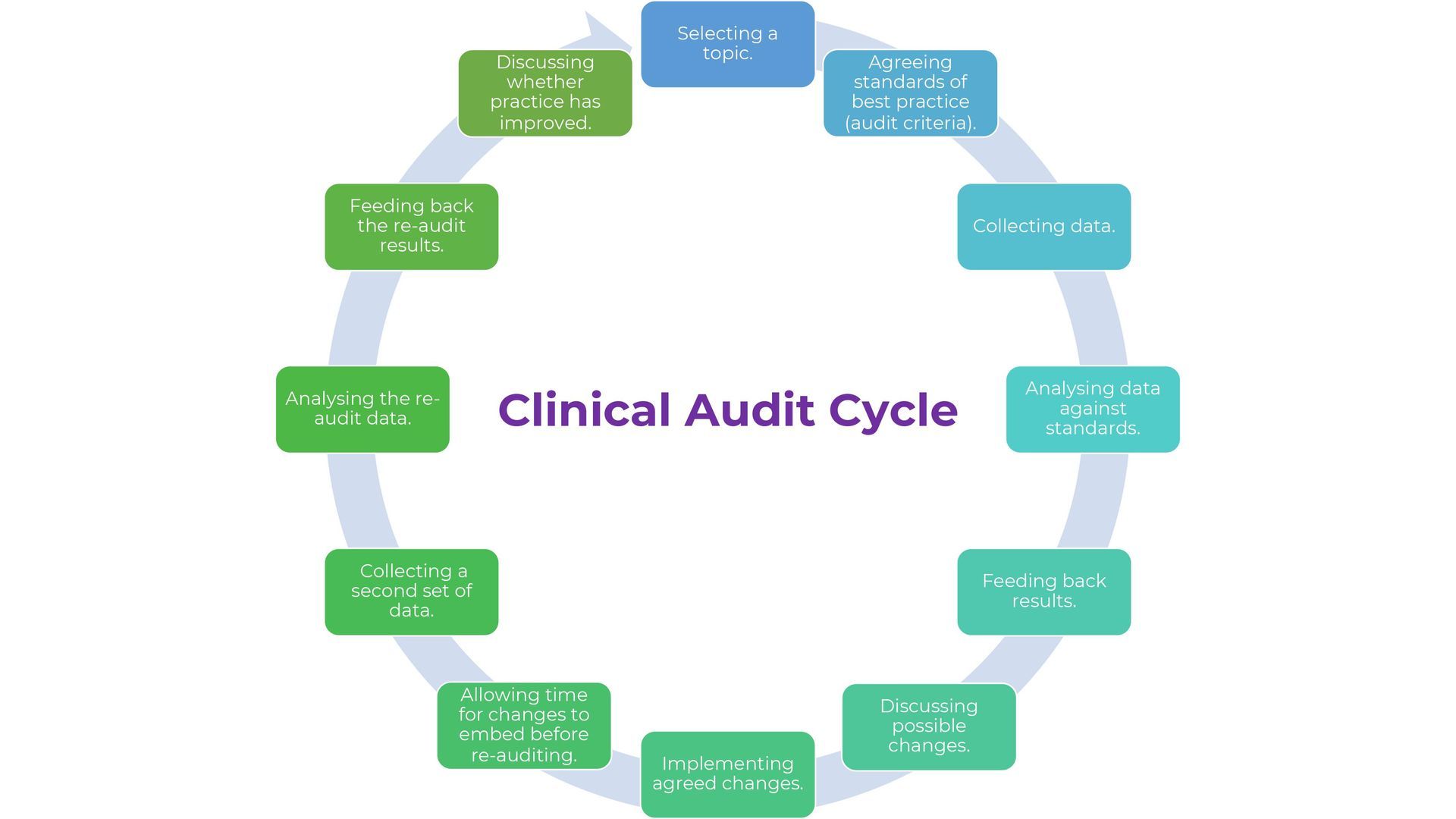
A health or social care setting where the entire team follows current standards and guidance underpins patient safety and is the goal for all care providers. With both the organisation and health and social care teams committed to providing 'Gold Standard' practice and safe care. Reducing preventable errors and avoidable complications may seem straightforward, this is not always the case when we are unsure of why errors,ommissions and non-compliance happen.
Implementing standards are beneficial
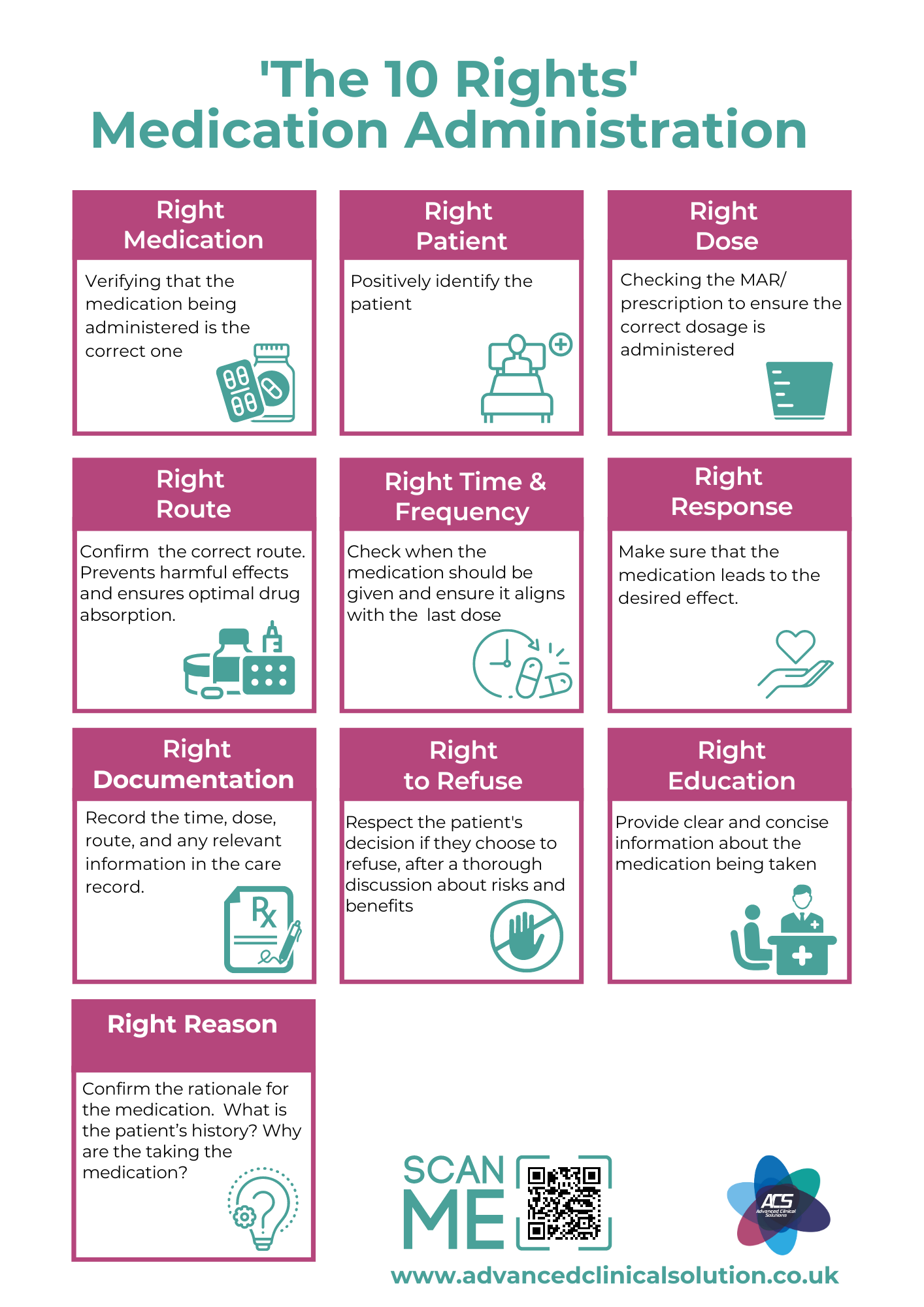
Much effort has gone into developing and sharing of evidence-based practice guidelines. Guidelines are "systematically developed statements'' to assist healthcare practitioners and patient decisions about appropriate actions to take in a given circumstance.
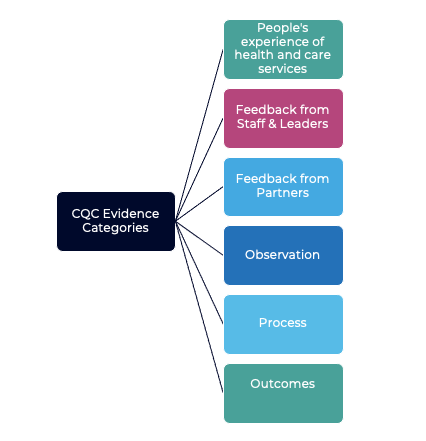
With so many organisations such as CQC, NICE, GMC and NMC to name a few releasing standards and guidance within the UK its clear implementing standards are beneficial: lowering overall costs, decreasing safety incidents, reducing preventable errors and improving service-user outcomes. Many updates are published each year, and the limited time available for searching and appraising the literature, evidence-based practice guidelines are usually been developed to assist health and social care workers in "best-practice" procedures. Although it has been shown that practice guidelines can improve quality of care. Whether this achieved in 'normal daily' practice remains unclear.
The barriers to achieving compliance can be challenging. Below are my top 6 questions to ask.1) Have we prioritised our workload ?
Too many and competing priorities. To action them all can be tough. Which priorities takes priority?
2.) Do we fully understand how to Implement?
Clarification and understanding of what the guidance and standards mean and how to action them in real terms.
3) Do we have the time and resources ?
Demands on healthcare workers time are high, time to keep abreast of new thinking and evidence can sometimes loose priority over essential patient care.
4) Who is responsible?
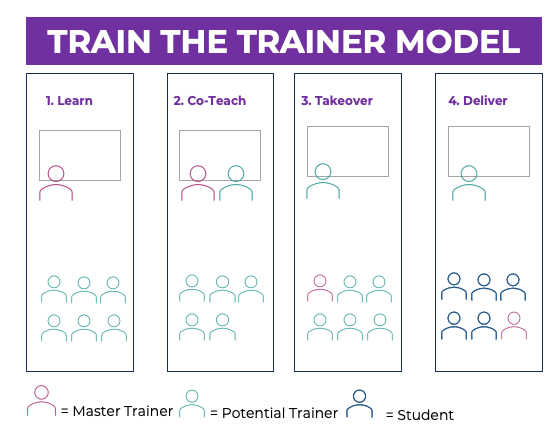
Clearly defined responsibilities over whose job it is to maintain practice guidelines and how information is disseminated to staff. This can sometimes be shared between dedicated educators and organisational managers.
5) Are we complacent ?
In any profession the day-to-day routine can lead to complacency about keeping up with developments in their specialism. In healthcare some issues are cultural e.g. 'we have always done it this way,' or 'this is how my senior has showed me how to do it'. Developing bad habits and cutting corners can often happen.
6.) Are we geared up for rapid change?
As different specialties advance quickly so too does the updated guidance and standards.
Achieving compliance with evidence-based practice guidelines will require an approach that takes into account practitioners' concerns about the complex nature of their work. Simply having evidence available does not mean that practitioners use it. Advanced Clinical Solutions provide support and assistance in improving compliance please contact us on 01633 415 427 or w www.advancedclinicalsolution.co.uk
Email Us
For general enquiries & questions,
contact us via email
Book Free Consultation
Need some advice face to face? Book a free 30 minute MS Teams consultation
Share
CHECK OUT OUR OTHER BLOG POSTS
Knowledge Hub