The Hawthorne effect :-Why staff may change their behaviour during an inspection
Identifying what behaviors change when staff and organisations are being inspected , and how this impacts on patient outcomes, may provide useful insights into how the quality of care can be improved.
The Hawthorne Effect is described as when individuals alter their behaviours in response to being observed.Healthcare stands among the professions that have adopted the technique of direct observation because it tends to reveal unexpected or even undesirable behaviours.
A study recently published in JAMA Internal Medicine , uncovered a unique form of the Hawthorne effect in healthcare organisations, with important consequences for patients.
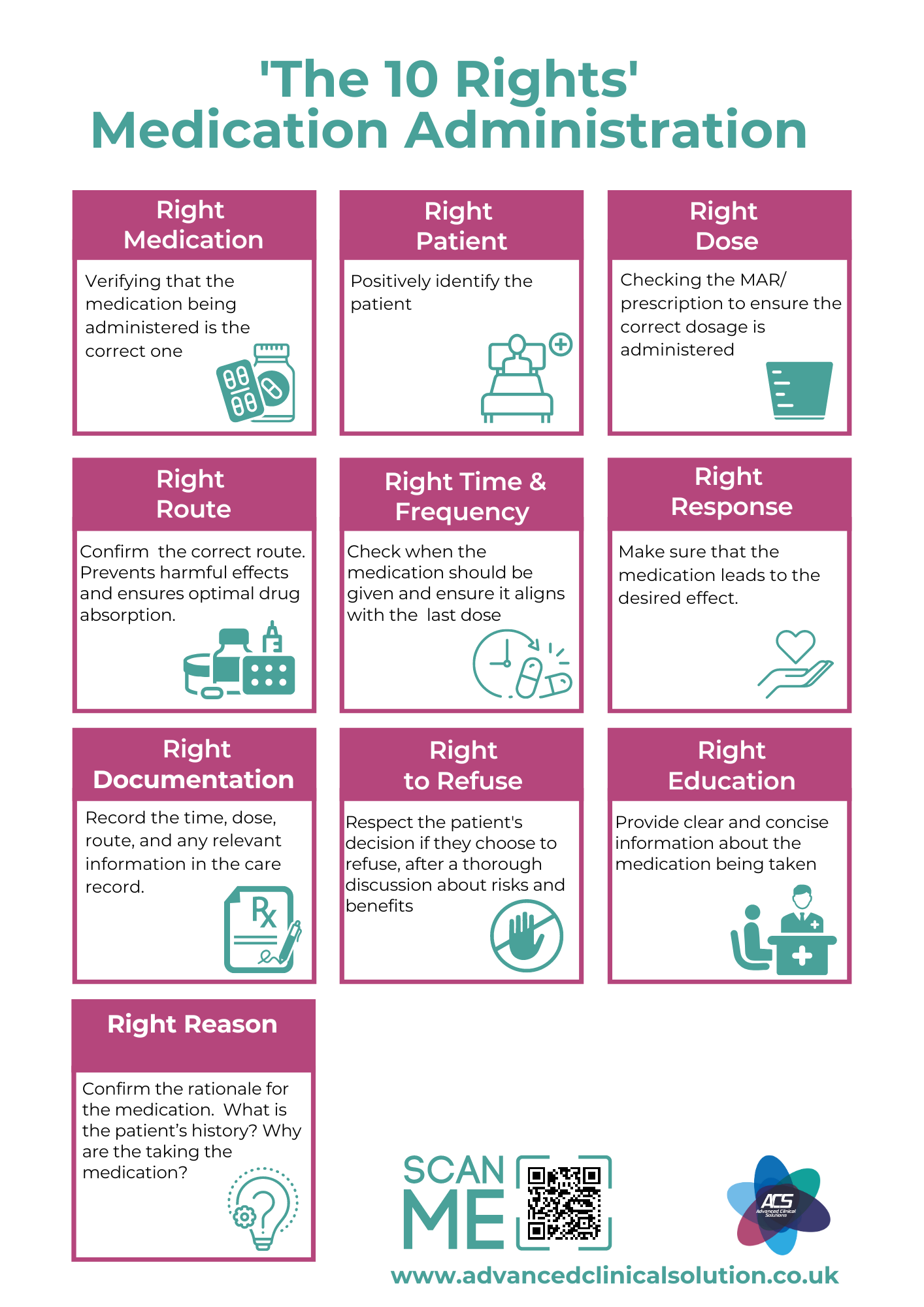
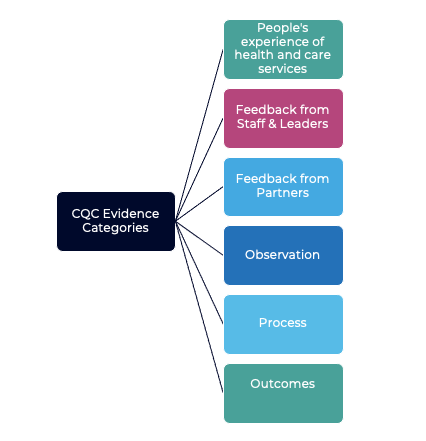
The study focused on and analysed how unannounced inspections affect patient outcomes. The inspections are done by the U.S. health care regulatory organisation in the study but bears many similarities to the English Care Quality Commission. To maintain registration, healthcare organisations are required to undergo unannounced, week-long inspections every 18 to 36 months. Again, very similar to CQC inspections as the focus is on adherence to a variety of quality and safety measures, including infection control practices, documentation and medicines management, to name a few.
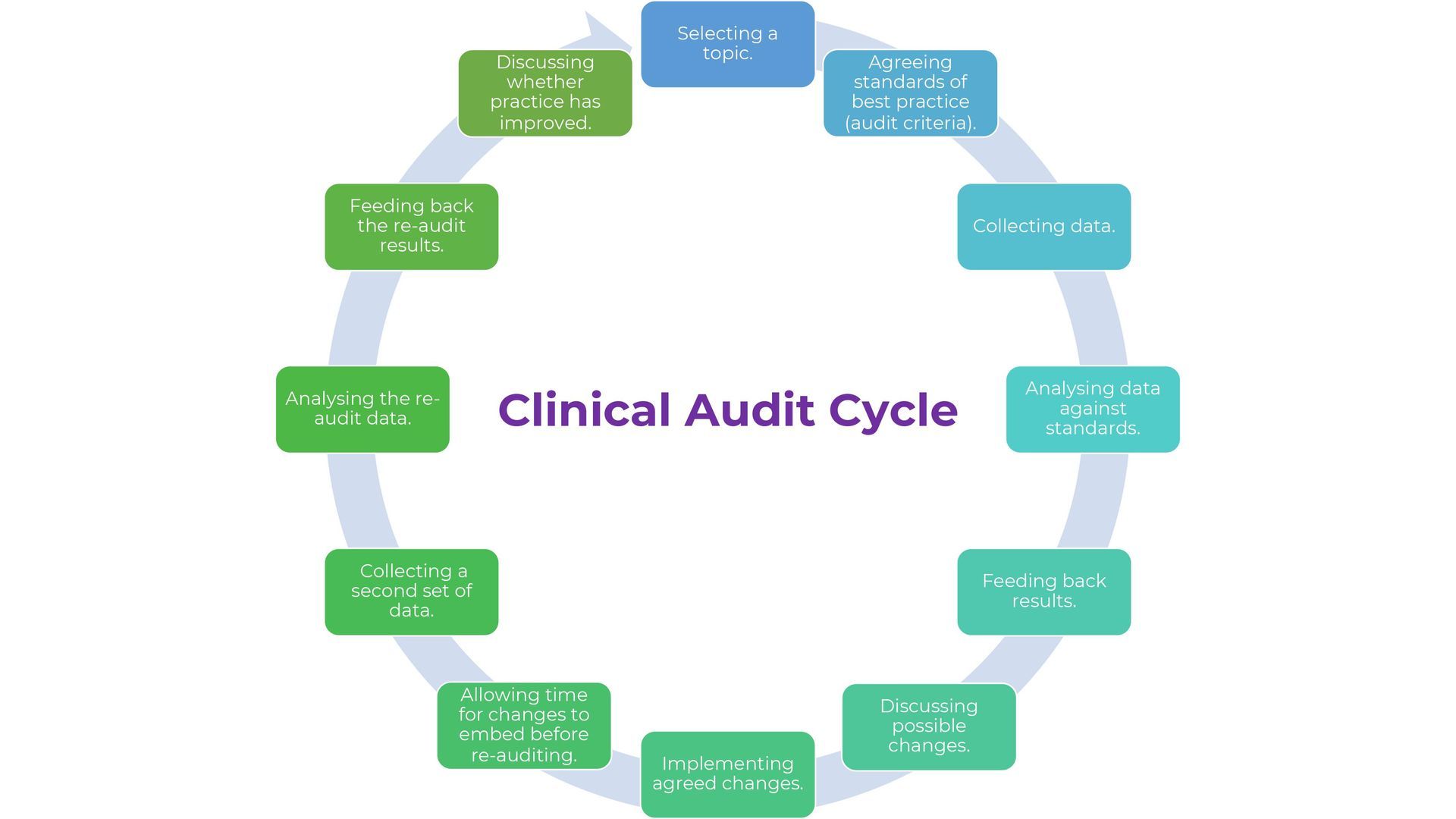
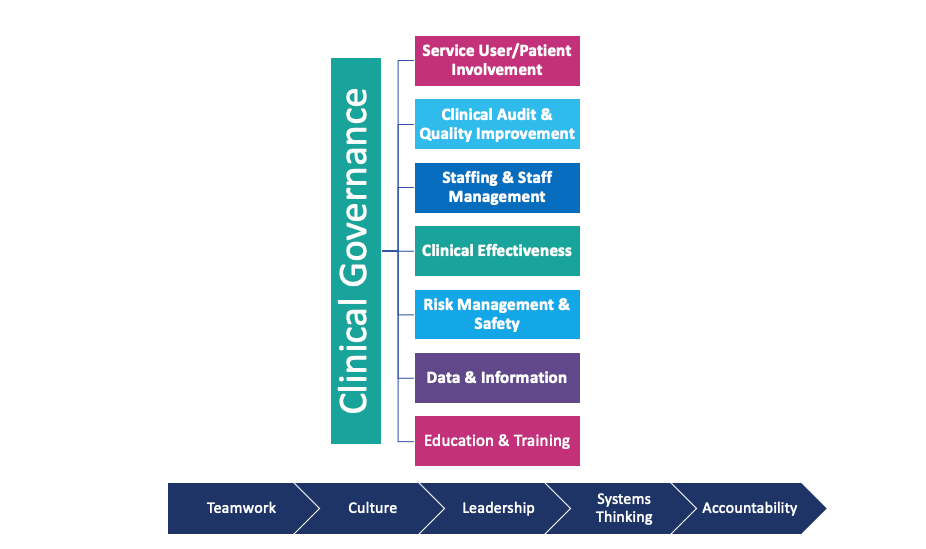
The pressure is high with little or no room for error – poor outcomes during the inspection process can harm an organisations reputation or even worse, force closure. It is inevitable that healthcare staff are overtly aware of their behaviour during the inspection period. It was also noted that healthcare organisations assemble huge amounts of resource to deal with inspections. Being involved within the healthcare sector for a long time I have experienced first-hand the inspection process which can be highly stressful. The most unflappable of people in an everyday situation crumble under the pressure. In more recent years I have been able to experience the other side of the coin by providing 'mock inspection' services as part of my clinical governance business.
Despite the level of attention these visits get, their immediate effect on staff behaviour and service user outcomes has not been explored in great detail.
One question to ask would be: Are patient outcomes during inspection and non-inspection periods are different?
Two possible explanations for why we see 'inspection effects' are interpreted.
-Healthcare staff may modify specific behaviours that are being measured, such as infection control practices, but there was no evidence that infection rates fell during inspection periods. It was also noted that other key measures such as pressure ulcers did not decrease either.
Is it also possible that healthcare staff were more focused during the inspection? Being open to criticism during visits may raise awareness of non-compliances and improve attention and vigilance – all of which would lead to better patient care, e.g. being more vigilant with documentation, which may give rise to better communication and in turn better quality of care. In addition, the mere presence of inspectors may reduce time spent by staff on non-work-related distractions.
How might the findings be used to improve patient care?
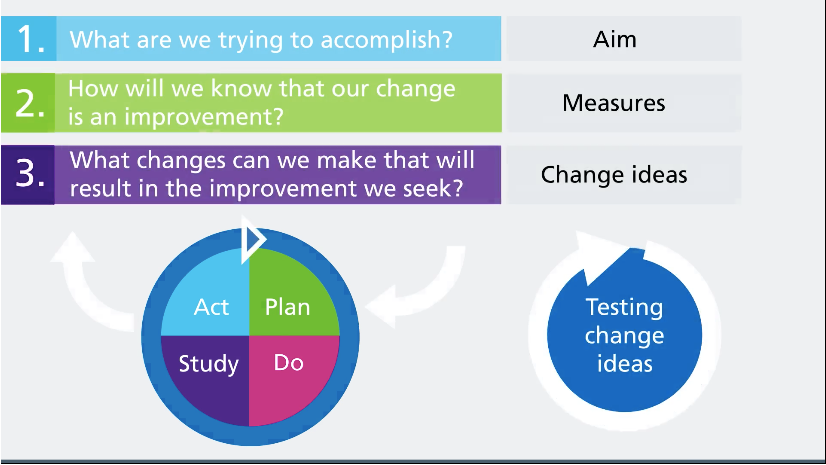
Healthcare organisations could observe which aspects of their day-to-day practices change the most to meet inspection standards. E.g. Is there evidence that infections fall? And is because handwashing increases? Identifying these changes may offer opportunities to improve care and patient outcomes.
Could increasing efforts to build attention and focus, into the normal workday by taking a systematic approach of the environment and other clinical human factors help? One example could be ensuring a ‘disruption’ free zone whilst giving medication.
To aid in inspection preparedness we offer 'mock inspections'
If you are keen to explore behaviours in an inspection scenario why not book a 'mock inspection' with us .For more information call 01633 415427 or visit www.advancedclinicalsolution.co.uk/services
Email Us
For general enquiries & questions,
contact us via email
Book Free Consultation
Need some advice face to face? Book a free 30 minute MS Teams consultation
Share
CHECK OUT OUR OTHER BLOG POSTS
Knowledge Hub